Through the Autism CARES Act of 2019, we improve care and outcomes for people with autism and other developmental disabilities (DDs).
We:
- Train health care providers and others to screen, refer, and provide services to children with autism and other DDs
- Use findings from our research programs to help people with autism and other DDs
- Make sure that states use best practices, including for children transitioning to adult services
2023 HRSA Autism Investments Across the United States
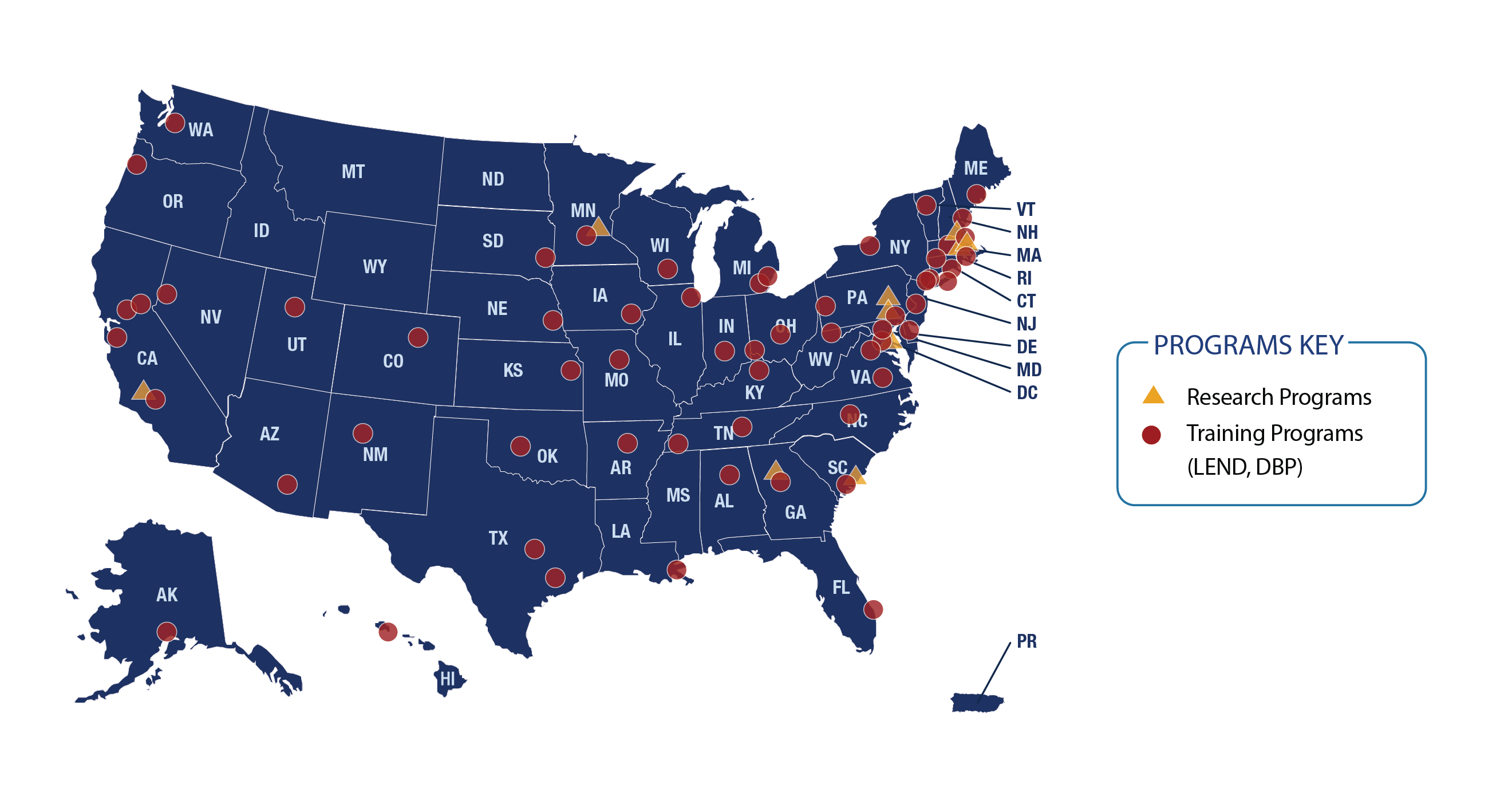
Image description
Map of the United States including Alaska, Hawaii, and Puerto Rico which shows the locations for Research Programs and Training Programs (LEND, DBP). Most states have at least 1 training program, with the exceptions of Idaho, Montana, Wyoming, and North Dakota, as well as Puerto Rico. Research Programs are in California, Minnesota, Georgia, South Carolina, Maryland, Pennsylvania, Massachusetts, and New Hamp-shire.
For a list of our current autism projects, visit these pages:
- Leadership Education in Neurodevelopmental and Other Related Disabilities (LEND) program
- Developmental-Behavioral Pediatrics Training Program (DBP)
- MCHB Research Investments
What makes HRSA’s autism programs unique?
Our programs make it easier for people to get the services they need.
We do this by:
- Training providers and collecting evidence to support our programs
- Conducting research and gathering data to understand how useful our interventions and strategies are
Every program includes feedback from people with lived experience. That helps us consider all aspects of their lives and make our programs effective for them.
Training the workforce
Our autism portfolio supports two training programs: LEND and DBP.
| Leadership Education in Neurodevelopmental and Other Related Disabilities (LEND) program | Developmental-Behavioral Pediatrics (DBP) Training program |
|
The LEND program:
In 2022,* there were:
In 2022, over 3,700 LEND faculty and trainees worked in clinical settings with historically underserved populations. LEND trainees and faculty provided 138,254 diagnostic services to verify or rule out autism or other DDs. For more information, read the LEND Fact Sheet (PDF - 369 KB). *Data from July 1, 2022, to June 30, 2023 |
DBP is a sub-specialty of pediatrics. It provides testing, counseling, and services for many children with developmental and behavioral issues and conditions. HRSA’s program supports a three-year DBP fellowship. The fellowship prepares fellows for leadership roles as teachers, researchers, and clinicians. It also helps medical students, residents, and practicing providers learn DBP skills. In 2021,** there were:
In 2021, 392 DBP faculty and trainees worked in clinical settings with historically underserved populations. DBP trainees and faculty provided 20,257 diagnostic services to verify or rule out autism or other DDs. For more information, read the DBP Fact Sheet (PDF - 502 KB). **Data from July 1, 2021, to June 30, 2022 |
Image description
“LEND was the highlight of my medical training. I was surprised we can graduate with-out LEND. The lived experience component was especially impactful. This makes sense as a way of learning, why don’t we have patients telling us about everything we are learning about? LEND changed the way I approach assessments. Now I think about how the report can support the family and the individual in many different con-texts. The language will follow them for the rest of their lives.” – Pediatrics Trainee, SUNY Stony Brook LEND
Our maternal and child health (MCH) training programs have a lifelong impact on the careers of MCH leaders. Read how trainees from our Developmental-Behavioral Pediatrics Training Program (PDF) described their experiences.
Conducting research
We fund studies and networks that focus on autism. The studies research the best ways to help children and youth with autism. Members of our Autism Research Networks share their findings by publishing peer-reviewed articles, developing clinical guidelines, and creating toolkits for audiences such as parents, caregivers, the community, and health care and service professionals.
In Fiscal Year 2022, our autism research investments supported 15 awardees at 72 sites, conducting 113 studies.
In Fiscal Year 2022, our Autism Research Networks and Autism Single Investigator Innovation Programs:
- Enrolled 10,191 participants in primary research studies
- Included over 1.3 million participants in secondary data analyses
Our autism research investments include:
- Autism Research Networks
- Autism Intervention Research Network on Physical Health (AIR-P)
- Autism Intervention Research Network on Behavioral Health (AIR-B)
- Developmental Behavioral Pediatrics Research Network (DBPNet)
- Healthy Weight Research Network for Children with Autism Spectrum Disorders and Other Developmental Disabilities (HWRN)
- Autism Single Investigator Innovation Program (SIIP)
- Autism Field-Initiated Innovative Research Studies (Autism FIRST)
- Autism Secondary Data Analysis Research (Autism SDAR)
To learn more, visit our research investments page.
Ensuring best practices for states and regions
Our programs create and advance national, state, and local level- strategies to support young people with autism or epilepsy as they transition from child- to adult-focused services. These plans are aligned with our Blueprint for Change, which helps children with complex health and social needs.
We promote partnership and collaboration between child and adult systems. We also encourage good communication between individuals with autism, their families, and their providers. Our goal is that young people with autism make a successful transition to adulthood in all aspects of their lives.
This year, we’re awarding a new demonstration program. It aims to improve the quality of life and well-being for youth with autism or epilepsy and their families or caregivers, as the youth transition from child- to adult-focused services.
Learn more about our Transition for Youth with Autism and/or Epilepsy Demonstration Projects and the National Coordinating Center on Transition.
Why are HRSA’s autism programs so important?
According to HRSA’s National Survey of Children’s Health, more than 2.2 million children 3 – 17 years old in the United States have autism.
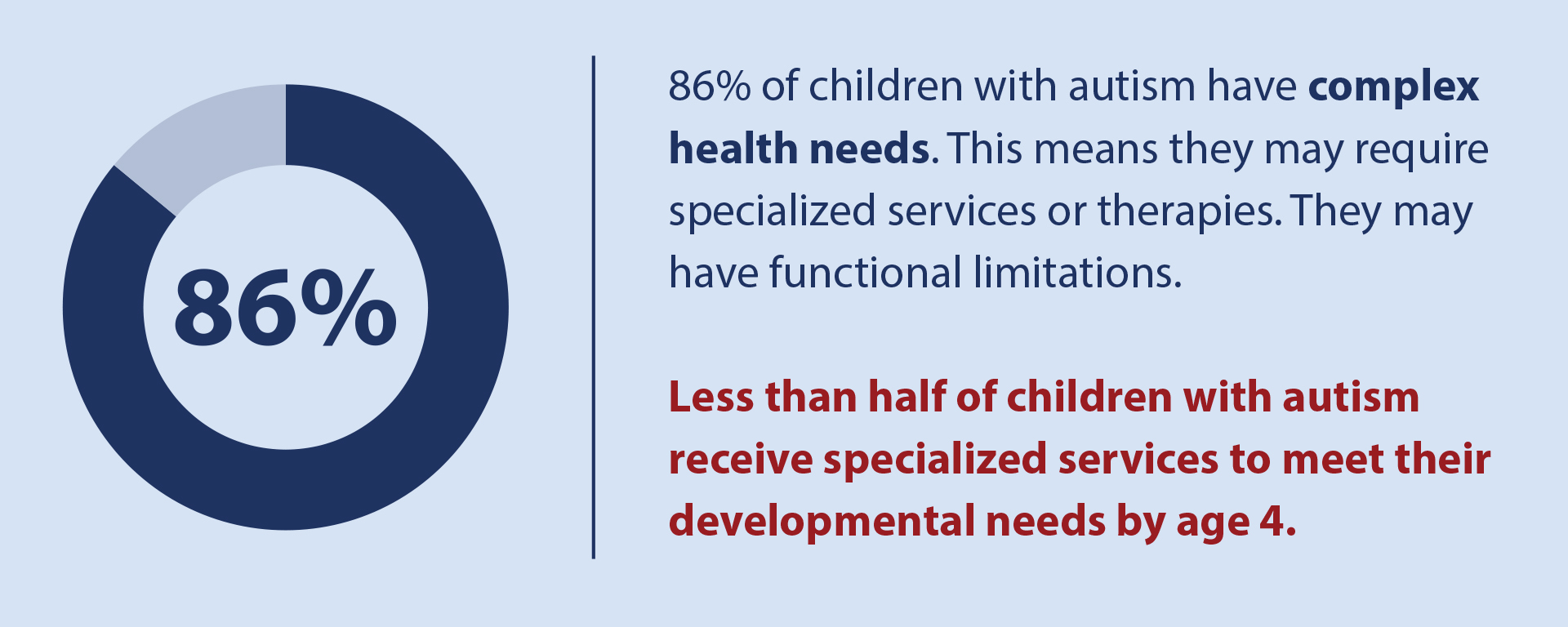
Image description
86% of children with autism have complex health care needs meaning they require the elevated need or use of specialized services, therapies, or they have functional limitations, but less than HALF of children with autism receive special services to meet their developmental needs by age 4.
Early screening, diagnosis, and services can improve a child’s development, symptoms, daily functioning, and quality of life.
What’s the history of these autism programs?
HRSA’s autism programs are authorized under Section 399BB of the Public Health Service Act. Congress first authorized these programs in 2008 and reauthorized them in 2011, 2014, and 2019. Congress must reauthorize these programs by September 30, 2024, for their activities to continue.
How HRSA coordinates autism efforts with other federal agencies
The Autism CARES Act also funds work in other Department of Health and Human Services (HHS) agencies like the Centers for Disease Control and Prevention and the National Institutes of Health.
HRSA works with other federal agencies to improve care for children and youth with autism and other DDs by participating on the Interagency Autism Coordinating Committee (IACC). The IACC coordinates all of HHS’ autism efforts.