Need assistance?
Are you a health care professional looking for help? Access consultation phone lines in ten states.
Are you a health care professional looking for help? Access consultation phone lines in ten states.
We fund this program to expand health care providers’ capacity to screen, assess, treat, and refer pregnant and postpartum people for mental health and substance use disorders (SUD).
Access our 2024 fact sheet (PDF - 144 KB) about this program.
We fund 13 awardees to carry out services in their state.
Read the closed notice of funding opportunity (HRSA-23-085).
Statewide programs are available in Colorado, Kansas, Kentucky, Louisiana, Missouri, Mississippi, Montana, North Carolina, Tennessee, Texas, Vermont, and West Virginia. There is also a regional program in Los Angeles County, California.
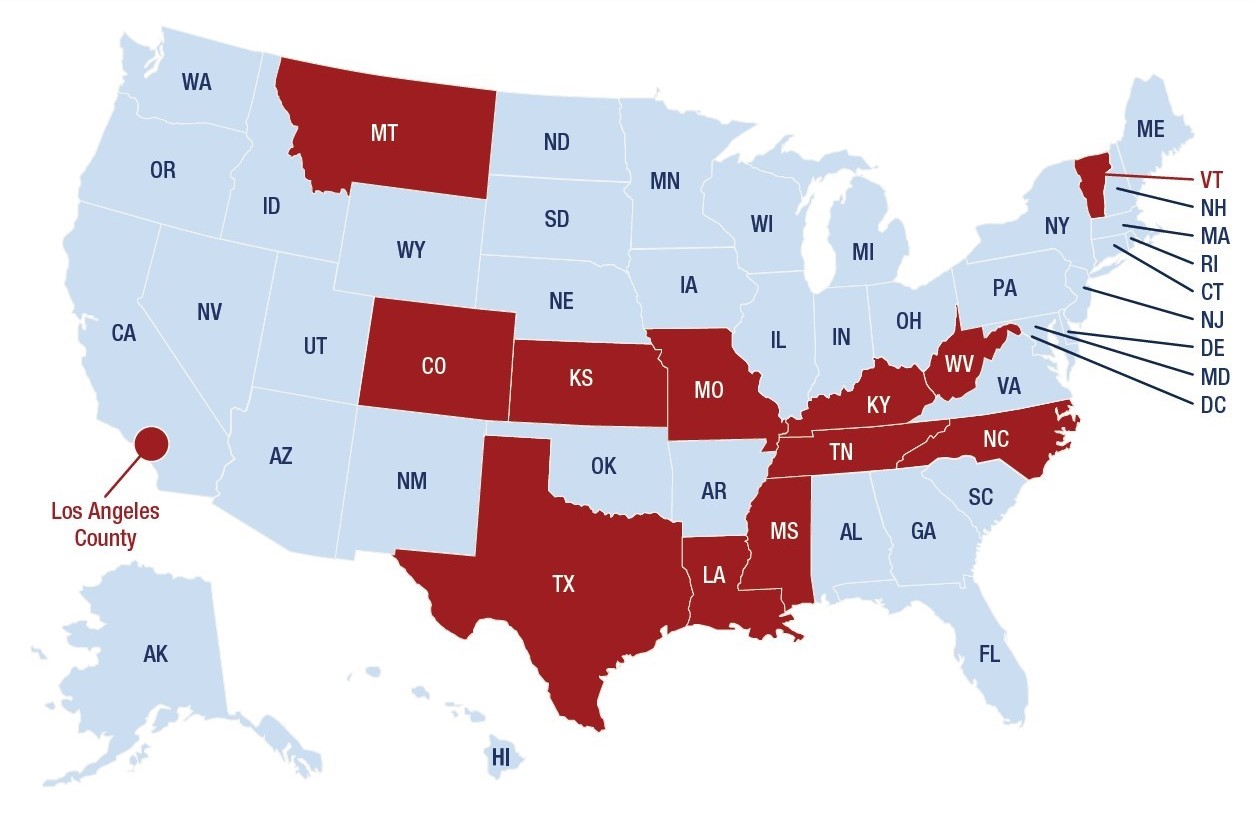
A map of the United States indicating which states and regions offer services and activities under the Screening and Treatment for Maternal Mental Health and Substance Use Disorders program.
States and regions that have Screening and Treatment for Maternal Mental Health and Substance Use Disorders services and activities: Colorado, Kansas, Kentucky, Los Angeles County, Louisiana, Mississippi, Missouri, Montana, North Carolina, Tennessee, Texas, Vermont, and West Virginia.
States that do not have Screening and Treatment for Maternal Mental Health and Substance Use Disorders services and activities: Alabama, Alaska, Arizona, Arkansas, California, Connecticut, Delaware, Florida, Georgia, Hawaii, Idaho, Illinois, Indiana, Iowa, Maine, Maryland, Massachusetts, Michigan, Minnesota, Nebraska, Nevada, New Hampshire, New Jersey, New Mexico, New York, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, South Carolina, South Dakota, Utah, Virginia, Washington, Wisconsin, and Wyoming.
Awardees provide front-line and maternal health care professionals with:
All training and services are:
Mental health conditions are the leading cause of pregnancy-related death, according to data from Maternal Mortality Review Committees in 38 states. This includes deaths due to suicide and drug overdose.
Depression is one of the most common complications during pregnancy and after childbirth. Research by the Centers for Disease Control and Prevention estimates 1 in 8 women are affected by postpartum depression.
According to data from the CDC’s Pregnancy Risk Assessment Monitoring System, depressive symptoms after childbirth are most commonly reported among:
This program:
Awardees collect and report data each year so that we know how many:
Learn about other programs we fund to address mental and behavioral health.
Looking for additional resources?
Stay up to date with MCHB: sign up for newsletters.
Find open positions with HRSA.